This patient cracked his molar biting a chicken bone. I was able to save the tooth, and without a root canal, but it did require a crown lengthening periodontal surgery and a crown.



This next patient bit down on a mint candy and fractured her molar down the root. The tooth could not be restored and was extracted and we will place a dental implant.


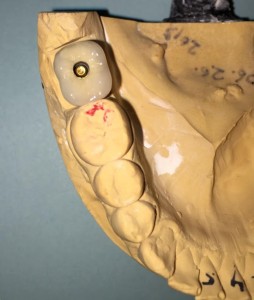
This was a challenging implant restoration case due to the alignment of implants. In order for the implant to osseointegrate firmly into the jaw bone we like to place the implants where the jaw bone is the thickest and strongest. In this case the best bone was not lined up nicely so we had to stagger the implants. I was still able to make the final implant crowns line up perfectly in the mouth.
Before and After
CBCT systems used by dental professionals rotate around the patient, capturing data using a cone-shaped X-ray beam. This data is used to reconstruct a three-dimensional (3D) image of the of the patient’s head and neck. CBCT uses more radiation than regular dental teeth x-rays, but still less than 10% of the radiation used in conventional medical CT scan of the same area.
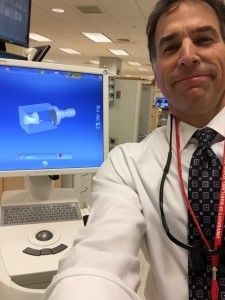
This is the Carestream 9300 Imaging machine we have at the University of Maryland Dental School. I mostly use this to plan dental implant placement.
Dentists use Cone Beam CT imaging for the following:• 3-D observation of overall oral/facial bony characteristics, allowing easier diagnosis and placement of dental implants • Surgical guide fabrication for implant placement • 3-D observation of teeth for endodontic diagnosis and treatment • Diagnosis and treatment of tooth impactions • Identification of inferior alveolar nerve and mental foramen location • Identification of the location of the maxillary sinus • Identification of the presence of odontogenic lesions • Trauma evaluation and treatment • Analysis of temporomandibular joint characteristics leading to diagnosis and treatment • Integration with CAD/CAM devices for fabrication of prosthodontics or orthodontic appliances • Identification for referral of numerous conditions or diseases not normally within the realm of dentistry, but that can be shown on typical cone beam images.
These last 2 pictures show how we use information obtained from the Cone Beam CT to plan placement of dental implants.
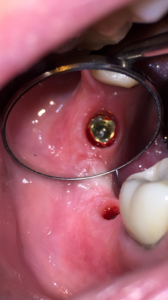
In this case report Dr. Gentry demonstrates the importance of taking a radiograph when seating the custom abutment and crown before final torquing of the gold implant interface connecting screw.


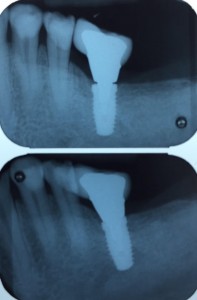



Here’s an example from a case I was doing with a dental student involving the 2 upper front teeth. In the first x-ray the impression copings were not fully seated. I re-positioned the copings and another x-ray was taken to confirm proper alignment. You cannot tell without an x-ray since this is below the gum-line.


Here’s an example of another implant check x-ray to verify proper seating.

To understand root canal treatment, it helps to know something about the anatomy of the tooth. Inside the tooth, under the white enamel and a hard layer called the dentin, is a soft tissue called the pulp. The pulp contains blood vessels, nerves, and connective tissue and creates the surrounding hard tissues of the tooth during development.
The pulp extends from the crown of the tooth to the tip of the roots where it connects to the tissues surrounding the root. The pulp is important during a tooth’s growth and development. However, once a tooth is fully mature it can survive without the pulp, because the tooth continues to be nourished by the tissues surrounding it
A root canal is necessary when the pulp, the soft tissue inside the root canal, becomes inflamed or infected. The inflammation or infection can have a variety of causes: deep decay, or a crack or chip in the tooth. In addition, an injury to a tooth may cause pulp damage even if the tooth has no visible chips or cracks. If pulp inflammation or infection is left untreated, it can cause pain or lead to an abscess.

Signs to look for include pain, prolonged sensitivity to heat or cold, tenderness to touch and chewing, discoloration of the tooth, and swelling, drainage and tenderness in the lymph nodes as well as nearby bone and gum tissues. Sometimes, however, there are no symptoms.
The dentist removes the inflamed or infected pulp, carefully cleans and shapes the inside of the root canal, then fills and seals the space. Afterwards, a crown or other restoration on the tooth to protect and restore it to full function. After restoration, the tooth continues to function like any other tooth.
Many root canal procedures are performed to relieve the pain of toothaches caused by pulp inflammation or infection. With modern techniques and anesthetics, most patients report that they are comfortable during the procedure.
For the first few days after treatment, your tooth may feel sensitive, especially if there was pain or infection before the procedure. This discomfort can be relieved with over-the-counter or prescription medications. Your tooth may continue to feel slightly different from your other teeth for some time after your root canal treatment is completed.
Root canal treatment can often be performed in one or two visits and involves the following steps:

1. The dentist examines and x-rays the tooth, then administers local anesthetic. After the tooth is numb, a small protective sheet called a “dental dam” is placed over the area to isolate the tooth and keep it clean and free of saliva during the procedure.

2. An opening in the crown of the tooth. Very small instruments are used to clean the pulp from the pulp chamber and root canals and to shape the space for filling.

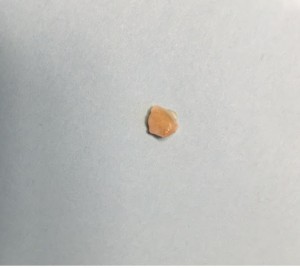
3. After the space is cleaned and shaped, the dentist fills the root canals with a biocompatible material, usually a rubber-like material called gutta-percha. The gutta-percha is placed with an adhesive cement to ensure complete sealing of the root canals. In most cases, a temporary filling is placed to close the opening. The temporary filling will be removed usually 1 week later.

Most teeth can be saved. Occasionally, a tooth can’t be saved because the root canals are not accessible, the root is severely fractured, the tooth doesn’t have adequate bone support, or the tooth cannot be restored.





CAD/CAM is an acronym for computer-aided design/computer-aided manufacturing. CAD/CAM technology has been increasingly incorporated into dentistry over the past 20 years. CAD/CAM technology is used by dentists and dental laboratories to provide our patients with 3-D milled ceramic crowns and other types of restorations, and to fabricate abutments for dental implants, used to replace missing teeth. A digital impression is taken of the patient’s teeth or dental impression, and the restoration is milled from a single block of tooth colored ceramic material in a milling chamber.


The 3-D milling machine fabricating the dental restoration.